A tooth infection might sound like a minor dental issue, but it can escalate into a life-threatening emergency if left untreated. In severe cases, a dental abscess can cause death within days, depending on the person’s immune system, the infection’s spread, and whether medical treatment is received. Understanding the timeline, symptoms, and dangers of untreated dental infections is crucial for early intervention and prevention of fatal complications – how long until a tooth infection kills you.
This article offers a medically grounded explanation of how tooth infections develop, how quickly they can become fatal, and what you should do to protect yourself. We present this topic with the seriousness it deserves, not as a scare tactic, but to inform and empower readers with facts that are often overlooked.
Understanding Tooth Infections: What Are They?
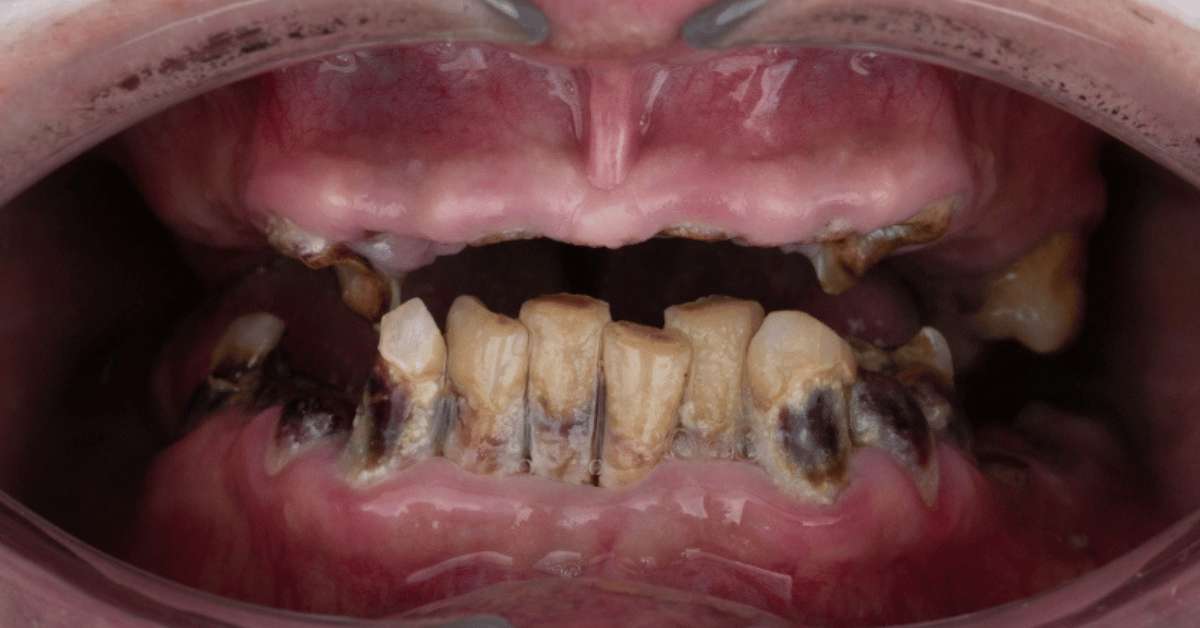
A tooth infection, or dental abscess, is a collection of pus caused by bacterial invasion of the dental pulp—the innermost part of the tooth that houses blood vessels and nerves. It usually starts from untreated cavities, failed dental work, gum disease, or trauma that allows bacteria to enter.
There are three primary types of tooth abscesses:
- Periapical abscess – Located at the tip of the tooth root.
- Periodontal abscess – Found in the gums, near the root.
- Gingival abscess – Confined to the gum tissue, often less dangerous.
The most dangerous are periapical and periodontal abscesses because they involve deeper structures and can more easily spread infection -how long until a tooth infection kills you.
How Infections Spread: The Hidden Danger
Bacteria do not remain localized if left untreated. They migrate. Initially, the infection is confined to the tooth or surrounding gum tissue. But over time, bacteria can invade the jawbone, sinuses, neck tissues, or even the bloodstream.
Pathways of Spread:
Oral region → Jawbone → Bloodstream → Organs (Heart, Brain, Lungs)
Once bacteria reach the bloodstream, the patient risks sepsis—a dangerous immune response to infection that can cause multi-organ failure and death within hours.
Critical Timeline: How Fast Can a Tooth Infection Kill?
While every individual case varies, below is a generalized timeline of how an untreated tooth infection can evolve into a deadly emergency.
Table: Timeline of Tooth Infection Progression
| Time Since Infection Starts | Stage Description | Symptoms | Risk Level |
|---|---|---|---|
| 0–3 Days | Localized Abscess | Toothache, swelling, sensitivity to hot/cold | Moderate |
| 3–7 Days | Tissue Spread | Fever, facial swelling, difficulty chewing | High |
| 1–2 Weeks | Facial Cellulitis | Throat or facial swelling, pain on opening mouth | Severe |
| 2–3 Weeks | Deep Neck Infection | Trouble breathing or swallowing, hoarse voice | Critical |
| 3+ Weeks (or sooner) | Systemic Spread (Sepsis) | Confusion, rapid heartbeat, drop in blood pressure, death | Life-Threatening |
Fatal Complications of Untreated Tooth Infections
When bacteria breach oral tissues and enter the bloodstream, a cascade of medical emergencies can follow.
1. Sepsis
Sepsis is the body’s extreme response to infection and is considered a medical emergency. If untreated, it can lead to septic shock and death within hours. Once organs begin to shut down, survival chances drop dramatically.
2. Ludwig’s Angina
This is a rapidly progressing cellulitis that affects the tissues of the floor of the mouth and neck. It can obstruct airways, causing death from asphyxiation.
3. Brain Abscess
If bacteria reach the brain via blood vessels or sinuses, a brain abscess can form. Symptoms may include seizures, altered consciousness, and death if untreated.
4. Endocarditis
An infection in the heart’s inner lining, most commonly affecting those with pre-existing heart conditions. It can cause permanent heart damage or death.
Warning Signs You Should Never Ignore
Some symptoms are clear indicators that a dental infection is no longer a minor issue:
- Persistent, severe toothache
- Facial swelling, particularly around the jaw, neck, or cheeks
- Fever higher than 101°F (38.3°C)
- Trouble swallowing or breathing
- Swollen lymph nodes in the neck
- Pus or foul taste in the mouth
- Red streaks spreading from the infected area (sign of blood poisoning)
If any of these symptoms appear, immediate medical attention is necessary.
Who Is Most at Risk of Death From a Tooth Infection?
Although anyone can develop complications, certain populations are at higher risk:
- Immunocompromised individuals (diabetes, HIV/AIDS, cancer patients)
- Elderly (reduced immune response)
- Young children (faster spread, difficulty communicating symptoms)
- People with poor access to healthcare
- Individuals who self-medicate or delay treatment
In many developing countries or underserved communities, untreated dental infections remain a silent cause of preventable deaths.
Misconceptions: Why Many People Underestimate the Risk
There’s a dangerous cultural misconception that tooth infections are “just dental issues.” Many believe antibiotics alone can fix the problem, or worse, rely on home remedies like saltwater rinses or clove oil for weeks.
However, antibiotics may only suppress the symptoms temporarily. Without physically removing the source—usually through drainage or root canal—the infection can rebound even more aggressively – how long until a tooth infection kills you.
Real-World Cases of Tooth Infections Leading to Death
Case 1: A 12-Year-Old Boy in Maryland (2007)
A young boy developed an abscess that led to a brain infection. Despite initial hospitalization, delays in dental intervention led to his death—a tragedy that spotlighted systemic issues in dental care access.
Case 2: A 26-Year-Old Man in California (2017)
He ignored a dental infection for over two weeks, thinking it would heal on its own. It spread to his lungs, and he died en route to the hospital.
These are not isolated cases. Deaths from dental infections still occur, especially when patients dismiss early signs or lack proper access to care.
Modern Treatment and Lifesaving Interventions
Once a tooth infection is diagnosed, treatment options vary depending on severity:
- Antibiotics: Used to reduce bacterial load but never replace drainage.
- Root Canal Treatment: Removes infected pulp and saves the tooth.
- Tooth Extraction: Necessary if the infection is severe or the tooth cannot be saved.
- Incision and Drainage: To relieve pressure and remove pus.
- Hospitalization: For intravenous antibiotics or surgery if the infection spreads.
Emergency Situations: When to Go to the ER
If you experience any of the following, go to the emergency room immediately:
- Swelling in the throat or difficulty breathing
- High fever with facial swelling
- Inability to open the mouth
- Confusion, dizziness, or low blood pressure
These are signs of sepsis, Ludwig’s angina, or deep neck infection—all potentially fatal if delayed – how long until a tooth infection kills you.
Preventing Tooth Infections: The Basics
Preventative dental care remains the best defense. Regular visits to the dentist can catch infections before they become dangerous.
Key Preventive Measures:
- Brush twice daily with fluoride toothpaste
- Floss regularly
- Avoid sugary snacks and drinks
- Visit the dentist every six months
- Don’t ignore cavities or cracked teeth
- Use antiseptic mouthwash if recommended
- Get prompt treatment for gum disease
Why Dental Infections Are Still Killing People in 2025
Despite medical advancements, deaths from dental abscesses continue due to:
- Misdiagnosis in early stages
- Socioeconomic barriers to dental care
- Antibiotic misuse leading to resistance
- Over-reliance on painkillers and home remedies
- Delayed emergency intervention
Public health campaigns rarely highlight the deadliness of dental infections. In most countries, dental health is treated separately from medical health, leading to dangerous gaps in care – how long until a tooth infection kills you.
What You Should Do If You Suspect a Tooth Infection
- Don’t delay. Even if the pain is tolerable, infections can escalate suddenly.
- Avoid self-medication. OTC drugs can mask pain but not cure the problem.
- Contact a dentist immediately. Request an emergency appointment.
- Monitor symptoms. Fever, swelling, or spreading redness means danger.
- Go to the ER if needed. A swollen throat, breathing difficulty, or confusion are medical emergencies.
FAQs
Q1: Can a tooth infection really kill you in a week?
Yes. If it spreads to vital areas like the brain or lungs or causes sepsis, death can occur in under a week.
Q2: Will antibiotics cure a tooth abscess permanently?
No. They may reduce symptoms but won’t eliminate the source. Dental procedures are needed.
Q3: Is facial swelling always a bad sign?
Yes. Swelling usually indicates that the infection has spread beyond the tooth.
Q4: What’s the difference between a regular cavity and a dental abscess?
A cavity is tooth decay. An abscess is an active infection with pus, pain, and serious risk.
Q5: Is it safe to wait until the pain gets worse before seeing a dentist?
Absolutely not. The longer you wait, the greater the risk of systemic infection and death.