Dental bone grafting has become one of the most significant advances in modern dentistry, allowing patients with bone loss to restore oral strength, improve implant success, and regain both functionality and aesthetics. In the simplest terms, a dental bone graft is a procedure where natural or synthetic bone material is placed in the jaw to build or restore bone that has been lost due to tooth loss, trauma, periodontal disease, or age. For patients seeking dental implants or stability in oral structures, bone grafting can be a vital first step. Within the first 100 words, it is essential to clarify that dental bone grafts are not only about improving appearance—they are critical for ensuring long-term oral health, enabling proper chewing, and preventing the collapse of facial structures. The procedure has become routine, widely accessible, and customizable, but understanding its process, benefits, and possible risks remains crucial for patients. This article explores every aspect of dental bone grafting in detail, addressing procedure types, healing timelines, alternatives, and future innovations.
What is a Dental Bone Graft?
A dental bone graft is a surgical intervention that supplements lost jawbone with bone material, encouraging natural regeneration and structural reinforcement. When teeth are lost, the surrounding jawbone begins to resorb because it no longer receives the stimulation that comes from chewing. This gradual reduction of bone can compromise adjacent teeth, alter facial appearance, and make it impossible to support dental implants without intervention. By placing graft material—whether from the patient, a donor, or a synthetic substitute—the body is stimulated to grow new bone around the grafted site. Over time, the graft material integrates, forming a stable base that restores oral function. The concept might sound modern, but bone grafting has been practiced for decades, evolving from primitive methods into today’s advanced, bioengineered procedures that prioritize safety, comfort, and predictability. Patients often undergo this treatment before dental implants, but it is equally valuable in cases of injury or severe gum disease where bone support is compromised.
Why is Bone Loss a Major Concern in Dentistry?
Bone loss in the jaw is one of the hidden but most serious challenges in dentistry. Unlike cavities, which can be immediately seen or felt, bone deterioration happens gradually and often without pain until the condition becomes severe. The jawbone plays a central role not just in anchoring teeth but also in maintaining facial structure and oral function. When bone shrinks, it leads to a sunken facial appearance, making individuals appear older. Furthermore, bone resorption reduces the stability of natural teeth, making them more prone to mobility and eventual loss. This spiral effect can trigger further bone loss, creating a cycle of oral decline. In patients who wish to receive implants, adequate bone volume is absolutely essential because implants require strong anchorage, similar to how roots secure natural teeth. Therefore, the introduction of dental bone grafts has transformed treatment planning, allowing dentists to provide implant solutions even to patients who would otherwise be deemed unsuitable due to insufficient bone structure.
Types of Dental Bone Grafts
Different types of dental bone grafts are available, each selected based on patient needs, source material, and specific oral conditions. Understanding these categories is essential to appreciate how personalized treatment can be.
| Type of Bone Graft | Source | Common Use | Key Benefit |
|---|---|---|---|
| Autograft | Patient’s own bone (e.g., chin, hip) | Large grafts or implant prep | Highest compatibility, no rejection |
| Allograft | Donor human bone (processed) | General use for implants | Readily available, safe, eliminates second surgery |
| Xenograft | Animal-derived (commonly bovine) | Long-term support | Strong scaffolding, gradual resorption |
| Alloplast | Synthetic (calcium phosphate, bioactive glass) | Smaller defects | Safe, no disease transmission |
Each type of graft comes with advantages and considerations. Autografts remain the gold standard due to biological compatibility, but synthetic and donor-based alternatives are becoming increasingly common, reducing patient discomfort and surgical complexity.
The Procedure: Step-by-Step Overview
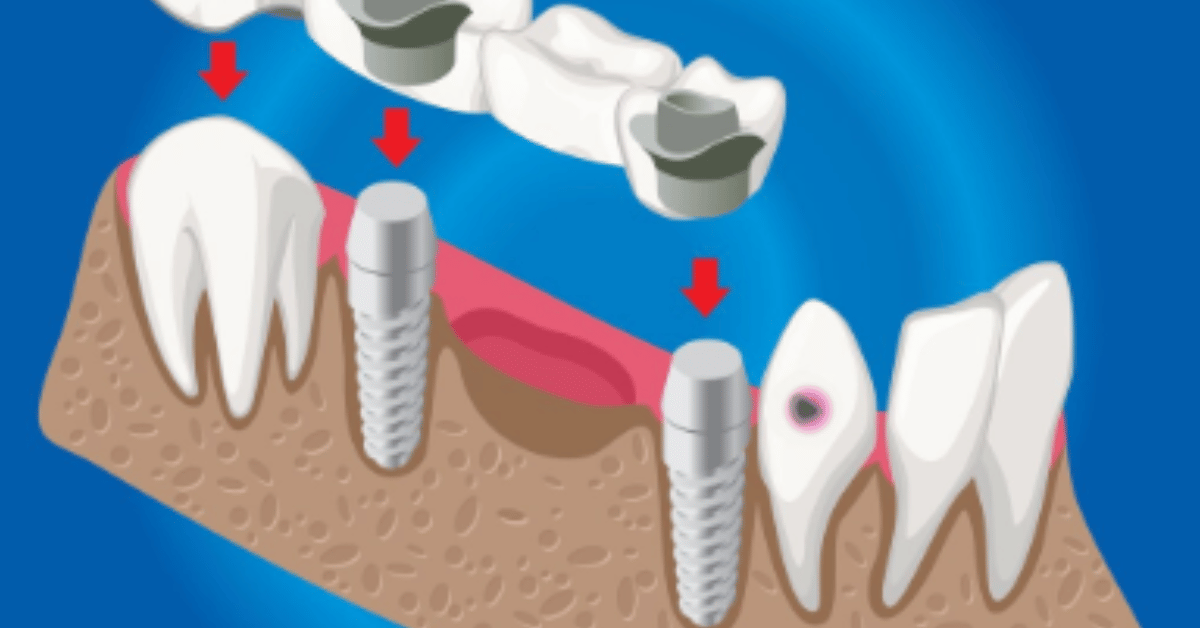
The process of dental bone grafting is typically performed by a periodontist or oral surgeon, often under local anesthesia with or without sedation. The procedure begins with a detailed diagnostic stage involving X-rays or 3D imaging to determine bone volume and defect location. Once a surgical plan is designed, the dentist makes a small incision in the gum to expose the bone. The grafting material is then carefully placed into the deficient area, sometimes combined with membranes that guide tissue regeneration and prevent soft tissue from interfering with bone growth. After placement, the area is closed with sutures and left to heal. Over the following months, natural bone integrates with the graft in a process called osseointegration. The duration of healing varies, typically ranging from four to nine months, depending on the size of the graft and the patient’s natural healing capacity.
Healing Process and Recovery
Recovery after a dental bone graft requires patience, as bone takes time to regenerate. Initial healing from surgery generally lasts about two weeks, during which swelling, mild discomfort, or bruising may occur. Patients are advised to avoid strenuous chewing, smoking, or activities that put pressure on the graft site. Pain is usually manageable with prescribed medication, and soft diets are recommended during the early healing phase. The most critical stage is the integration of graft material with the natural bone, which can take several months. Follow-up appointments with imaging allow dentists to monitor progress and ensure successful regeneration. Unlike fillings or crowns, which deliver immediate results, bone grafting is a foundation-building procedure—its success is measured over time by the stability it provides for future restorations such as implants. “Good dentistry is not just about repairing teeth but about rebuilding what supports them,” as one oral surgeon described the philosophy behind bone grafting.
Benefits of Dental Bone Grafts
Dental bone grafting offers a wide spectrum of benefits that extend far beyond implant preparation. One of the most significant advantages is the restoration of jawbone volume, which preserves facial contours and prevents premature aging associated with bone resorption. Another benefit lies in functional improvement; a strong jawbone allows individuals to chew food properly, enhancing digestion and overall health. Bone grafts also stabilize neighboring teeth, reducing the risk of further loss. Psychologically, patients gain confidence knowing their oral health is being rebuilt from the ground up. In terms of implants, grafting dramatically improves success rates, offering reliable support for artificial roots. As one patient shared, “I didn’t just regain a smile, I regained the ability to enjoy food and conversation without worry.” For many, the treatment represents more than a surgical solution—it is a life-enhancing procedure that bridges the gap between dental necessity and overall well-being.
Risks and Considerations
Despite its benefits, dental bone grafting is not without potential complications. Patients may experience infection, graft rejection, or failure of integration, although these risks are relatively rare with modern techniques and materials. Swelling and mild pain are common but temporary. Another consideration is cost, which varies depending on graft type, surgical complexity, and whether additional procedures such as sinus lifts are required. Insurance coverage is inconsistent, often depending on whether the graft is deemed medically necessary. Additionally, healing time can be a deterrent for patients eager for immediate implant placement. Understanding these factors helps individuals make informed decisions about their oral health journey. Dentists often emphasize transparency during consultation, ensuring that patients know both the strengths and limitations of bone grafting. The key to minimizing risks lies in proper case selection, skilled execution, and adherence to post-operative care instructions.
Alternatives to Dental Bone Grafting
While bone grafting is the gold standard for rebuilding lost jawbone, several alternatives exist, depending on the degree of bone loss and patient suitability. Techniques such as distraction osteogenesis stimulate natural bone growth by gradually separating bone segments, encouraging new tissue to form. Ridge expansion is another approach, widening a thin jawbone to make room for implants. In some cases, short or angled implants are used as an alternative, bypassing the need for grafting altogether. These alternatives highlight how dentistry has advanced to provide multiple pathways for restoring oral function. However, none match the predictability of bone grafting when substantial bone volume is missing. The decision between a graft and alternatives depends on clinical evaluation, patient preferences, and long-term goals.
Cost Factors and Patient Considerations
The financial aspect of dental bone grafting is often a decisive factor for patients. Costs vary widely, typically ranging from a few hundred dollars for minor synthetic grafts to several thousand for extensive autografts involving hospital stays. Factors influencing cost include graft material, diagnostic imaging, anesthesia, and additional procedures like sinus lifts. Geographic location and dentist expertise also play roles in pricing. Insurance may cover bone grafting if it is tied to trauma or medical necessity but often excludes elective grafts for implants. Patients should discuss financing options and clarify coverage with their providers. Importantly, the long-term benefits often outweigh the initial expense, as bone grafting lays the foundation for durable restorations.
Comparative Healing Times
| Graft Type | Average Healing Time | Suitability for Implants |
|---|---|---|
| Autograft | 4–6 months | High success, ideal for implants |
| Allograft | 6–9 months | Reliable, slightly longer integration |
| Xenograft | 6–12 months | Long-term stability, gradual absorption |
| Synthetic | 4–9 months | Safe, variable success rates |
Healing times illustrate how patient expectations must align with biological realities. Faster healing is possible with autografts, but synthetic options reduce surgical invasiveness, offering a trade-off between convenience and duration.
Future of Dental Bone Grafting
The future of dental bone grafting is shaped by biotechnological innovation and regenerative medicine. Researchers are developing stem-cell-enhanced grafts that stimulate faster bone growth and reduce healing time. 3D-printed graft materials tailored to a patient’s anatomy promise higher precision and better outcomes. Growth factors, such as bone morphogenetic proteins, are already being tested to accelerate integration. These innovations could eventually make bone grafting less invasive, more predictable, and significantly faster. Dentistry is moving toward biologically intelligent solutions, where the body is guided to heal itself with minimal external intervention. As one researcher put it, “We are not just filling spaces with material; we are programming biology to rebuild.” For patients, this means a future where bone loss may no longer be an obstacle to implants or oral rehabilitation.
Conclusion
Dental bone grafting is more than a surgical procedure—it is a cornerstone of modern dentistry that enables patients to regain function, confidence, and quality of life. From understanding bone loss to exploring graft types, risks, and future innovations, patients today are better equipped to make informed choices about their oral health. While costs and healing times require consideration, the long-term stability and benefits often outweigh these challenges. Importantly, dental bone grafting represents the synergy between science and healing, where technology and biology come together to restore what time or disease has taken away. As dentistry continues to evolve, patients can expect even more refined solutions, ensuring that the foundation of oral health remains strong. To borrow the words of a renowned oral surgeon, “In rebuilding bone, we are not just restoring a smile—we are restoring life’s most fundamental functions.”
FAQs
1. How long does it take for a dental bone graft to fully heal before implants can be placed?
The healing period depends largely on the type of graft material used, the size of the defect, and individual biology. On average, healing may take anywhere from four months to a year. Autografts, because they come from the patient’s own bone, tend to integrate faster, often within four to six months. Donor or synthetic grafts usually require longer integration, sometimes up to nine or twelve months. During this time, the graft hardens and fuses with existing jawbone. Only when sufficient stability is confirmed through X-rays or 3D scans will dentists move forward with implant placement, ensuring maximum success rates.
2. Is a dental bone graft painful, and what can patients expect after surgery?
Most patients are pleasantly surprised at how manageable the discomfort is after a bone graft. The procedure is performed under local anesthesia, and sometimes sedation, ensuring no pain during surgery itself. Post-operatively, swelling, minor bruising, and tenderness are normal but usually subside within a week or two. Pain relief is typically achieved with over-the-counter medication, although stronger prescriptions may be provided for larger grafts. Patients are advised to follow a soft diet, maintain careful oral hygiene, and avoid smoking or strenuous activity. With proper care, discomfort is temporary and outweighed by the long-term benefits of restored bone health.
3. Who is an ideal candidate for a dental bone graft procedure?
Candidates include individuals who have lost teeth and experienced jawbone resorption, patients with gum disease that weakened supporting bone, or those preparing for dental implants but lacking sufficient bone structure. Trauma victims and patients with congenital jaw deficiencies also benefit. Good overall health is vital, as conditions like uncontrolled diabetes, smoking, or immune suppression can interfere with healing. A comprehensive dental and medical evaluation determines candidacy. In some cases, smaller grafts can be placed simultaneously with implants, but most patients require staged treatment to ensure predictability and success.
4. Are there risks of infection or rejection with bone grafting?
While bone grafting is considered safe and predictable, risks are possible. Infection at the surgical site is the most common but is generally preventable with antibiotics and proper care. Graft “rejection,” in the traditional sense, is rare since materials are either biocompatible or harvested from the patient’s own body. More commonly, failure occurs if the graft does not integrate fully with the existing bone. Factors like smoking, poor oral hygiene, or systemic illness increase risk. Regular follow-ups allow early detection of issues, and with today’s sterilization standards and advanced biomaterials, serious complications remain uncommon.
5. How much does a dental bone graft cost, and does insurance cover it?
The cost varies widely, depending on graft type and complexity. Small synthetic grafts may cost a few hundred dollars, while autografts requiring hospital surgery can exceed several thousand. Additional costs for anesthesia, imaging, and membranes can add to the final bill. Dental insurance coverage is inconsistent; many plans cover bone grafting if it is linked to trauma, disease, or medically necessary reconstruction. However, elective grafts done solely to prepare for implants are often excluded. Patients should consult both their dentist and insurance provider to clarify coverage, while also exploring financing or payment plans offered by clinics.